We all know that human blood is red, does leukemia mean that the blood becomes “white”? In leukemia, the blood does turn “white”, but instead of turning white to the naked eye, there is an abnormal increase in the number of white blood cells, which is why it is called leukemia. These abnormally increased white blood cells are usually underdeveloped and are therefore called bud cells or leukemia cells. The picture below shows a leukemia bud cell observed under a microscope.
Where do these abnormal bud cells come from?
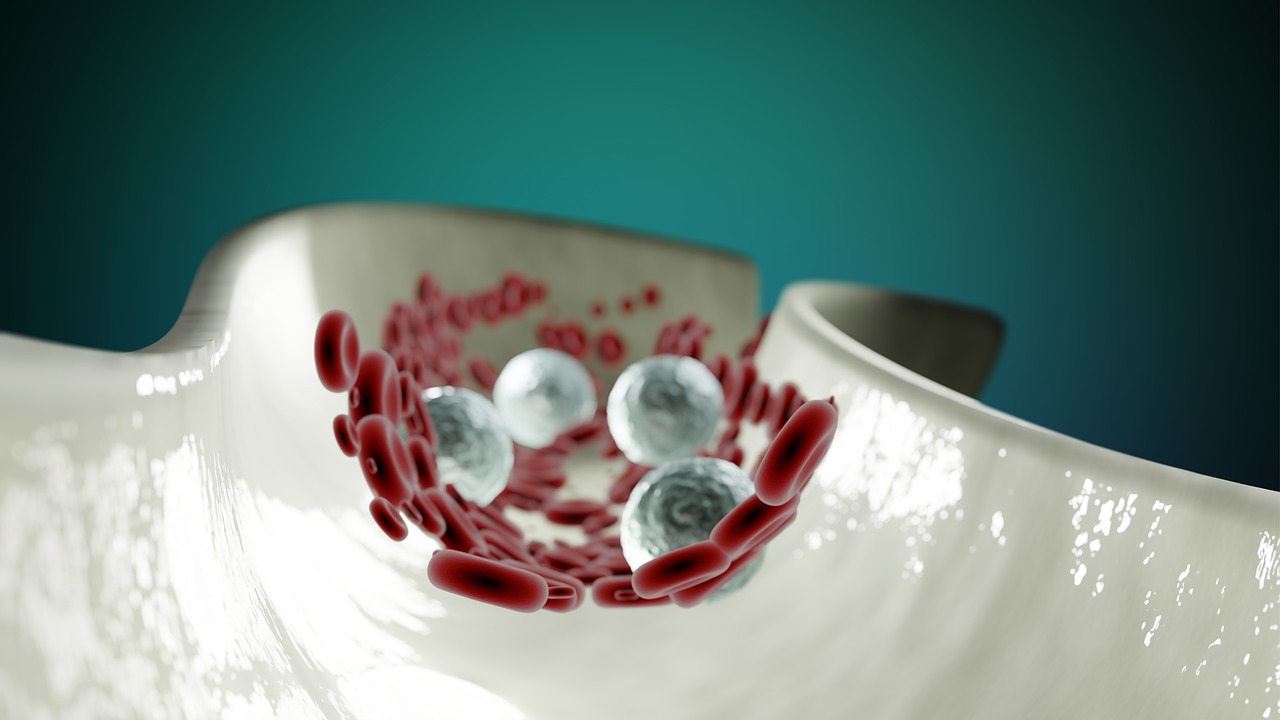
Leukemia, also known as blood cancer, usually occurs in the bone marrow because the blood cells in the blood originate from the bone marrow and are differentiated from the hematopoietic stem cells in the bone marrow. As we can see from the diagram of blood cell differentiation below, in leukemia, there is a problem with the differentiation of the bone marrow stem cells into bone marrow blast cells and then into various types of white blood cells. As a result, a large number of abnormal bone marrow blast cells accumulate in the patient’s bone marrow, which then spreads to the patient’s bloodstream, signaling the disease.
What are all the symptoms of leukemia?
Patients with leukemia may experience symptoms caused by the destruction of the hematopoietic function of the bone marrow due to the accumulation of abnormal cells in the bone marrow. As the white blood cells penetrate into the tissues, the patient may also experience symptoms caused by the penetration of white blood cells into the tissues. Symptoms of myelopoiesis include anemia, persistent fever, susceptibility to infections, and a tendency to bleed in spots. These symptoms are due to the lack of platelets and red blood cells, decreased immunity, and susceptibility to infections as a result of the destruction of bone marrow hematopoiesis. Symptoms caused by white blood cells penetrating the tissues are, on the other hand, enlarged lymph nodes, bone or joint pain, swollen gums, bleeding gums, enlarged liver and spleen, and pericardial effusion. Of course, these symptoms are the clinical symptoms that may appear after the diagnosis of leukemia, it does not mean that the appearance of these symptoms is the precursor of leukemia. Once you notice any abnormality in your body, make sure you do a clinical examination and let the doctor make a judgment instead of making a judgment on your own based on the written description of the disease, scaring yourself, or even making a mess.
What are the causative factors of leukemia?
Unfortunately, the exact cause of leukemia is still unknown. It is currently believed that environmental and genetic causes are the main causes of the disease. Environmental causes of leukemia occur when a patient is exposed to disease-causing agents in the environment that can cause DNA mutations in bone marrow stem cells. These causative agents are usually radiation (e.g., radiation, chemotherapy, etc.), carcinogens (e.g., smoking, chemicals such as benzene, etc.), and so on. Genetic predisposition is the possibility that the patient may have a family history of leukemia, Down syndrome, etc.
How do you treat leukemia?
Although leukemia is known as “blood cancer”, it is not a terminal disease. With the right treatment, the clinical cure rate of leukemia can be as high as 70%.
Treatments for leukemia include chemotherapy, radiation therapy, targeted therapy and bone marrow transplantation. Chemotherapy is the use of drugs to kill leukemia cells or slow down the growth and division of leukemia cells; radiotherapy is the use of X-rays or gamma rays to cut down or kill leukemia cells; targeted therapy is the use of biological drugs to specifically attack leukemia cells and inhibit their growth; bone marrow transplantation is the use of anticancer drugs to kill leukemia cells in the body of the patient, and then inject healthy bone marrow donated into the body of the patient, so that normal and healthy bone marrow cells can start to grow and develop in the patient. Bone marrow transplantation involves using anti-cancer drugs to completely kill the leukemia cells in the patient’s body, and then injecting the donated healthy bone marrow into the patient’s body to allow the normal healthy bone marrow cells to begin to differentiate into normal blood cells. The cure rate of leukemia depends on a number of factors, including the type of diagnosis, the age of the patient, and his or her condition. The cure rate for acute lymphoblastic leukemia (ALL) treated with chemotherapy is 60-70%, with a 5-year survival rate of 89% for young children and adolescents under 20 years of age, and about 35% for adult patients 20 years of age and older.
When patients with acute myelogenous leukemia (AML) are treated, the 5-year survival rate for adolescent and child patients under 20 years of age can be 67%, while the 5-year survival rate for adult patients 20 years of age and older is about 24%. Bone marrow transplantation therapy improves the cure rate for AML patients. Chronic lymphatic leukemia (CLL) is common in Western countries and chronic myelogenous leukemia (CML) is common in Asian countries. Compared to acute leukemia, chronic leukemia progresses slowly and patients with chronic leukemia can still survive for an additional 3-5 years without bone marrow transplantation.
Is leukemia hereditary?
Theoretically, leukemia is generally not hereditary, and the majority of confirmed clinical cases occur in patients without any family history of leukemia. Of course, there are some cases where a close family member with a diagnosis of leukemia may develop the same type of leukemia. However, since the cause of leukemia has not yet been identified, it cannot be definitively concluded that a diagnosis of leukemia will be passed on to future generations. Similarly, the diagnosis of the same type of leukemia in a close relative does not exclude the possibility that similar living conditions led to the diagnosis.
How can I take care of a person with leukemia who is close to me?
Leukemia patients undergoing chemotherapy are usually prone to oral problems, such as ulcers on the oral mucosa, bleeding in the mouth, gastrointestinal tract, and skin due to platelet drop. Therefore, caregivers need to pay attention to help patients rinse their mouth with saline or mouthwash with pain relief function. At the same time, due to the decline in immunity of leukemia patients after treatment, caregivers need to pay special attention to the environmental hygiene of the patient’s surroundings, avoiding the patient’s access to public places, and reminding the patient to wear a mask when going out. Finally, caregivers should always pay attention to whether the patient takes medication regularly and undergoes regular checkups.